Endocrine Glands |
|||
| Atlas: | |||
| Text: | |||
Overview: The goal of this lab is to examine and describe the cellular organization of the major organs of the endocrine system. Below is a short summary of the nomenclature, key structural features, and main hormones of each organ.
Slide DescriptionsWebslide Hypohysis_A: Pituitary (Hypophysis), human, H&E (courtesy of Univ. Tasmania) [DigitalScope] This is a slide of the human pituitary stained with H&E. By eye, note the overall shape of the gland and the conspicuously different staining properties of the pars distalis (anterior lobe or adenohypophysis) and the pars nervosa (posterior lobe or neurohypophysis). At low power, survey the section. Note the glandular nature of the pars distalis (compact cords of cells, highly variable in their staining, remarkably well supplied with broad capillaries). Contrast this with the fibrous, poorly staining posterior lobe. At high power, survey the anterior lobe trying to find a region showing good staining and preservation. You should be able to find several good examples of the three classical cell types of the pars distalis: Acidophils are the most abundant class. They are small with densely red cytoplasm. Basophils have pale staining nuclei and dark purple granules in their cytoplasms. Chromophobes can be recognized as the cells with the most pale-staining cytolasms. Reticular fibers divide the gland into nests, surrounded by capillaries. Are the cell nests type-specific? The neural lobe has two cellular elements, very fine axons of hypothalamic neurons which have passed down the infundibulum to enter the pituitary, and, pituicytes. The latter are neuroglia; only their oval nuclei are seen. Their cell processes are not apparent in this preparation. Dilations of the axon terminals filled with neurosecretory material, called Herring bodies, cannot be reliably demonstrated in this slide. Sandwiched in between the pars distalis and pars nervosa is the pars intermedia, which in humans consists of a small collection of basophil cells and a trail of small Rathke's cysts that are remnants of Rathke's pouch.
Webslide 0050_F: Thyroid Gland, monkey, 1.5 um, H&E [DigitalScope] At low power, note the shape of the follicle epithelial cells and the relative volume of colloid to cells. How would you characterize this monkey's thyroid status? (Note: the occasional "islands" of cells seen within the colloid of some follicles in this specimen are either grazing sections of folicular cells seen en face and/or cells that have sloughed off during preparation). Large granules are sparsely present in the follicle cells. What hormone do they contain?
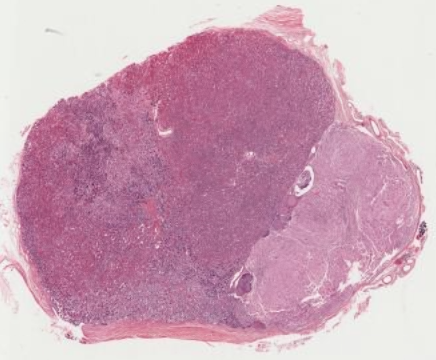
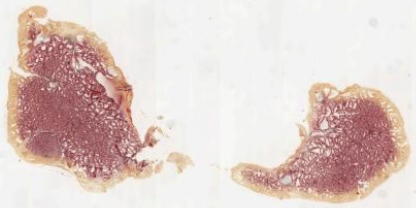
Webslide 0052_F: Thyroid-Parathyroid, young mammal, H&E. Paraffin [DigitalScope] This thyroid gland was in a euthyroid state, as judged by the cuboidal epithelium. Note the abundant cytoplasmic granules. The rich capillary bed about each follicle is not evident but occasional capillaries with RBCs can be seen in longitudinal sections. The colloid is artifactually shrunken; compare with WebSlide 50. The parathyroid gland is the small, cellular body attached to the thyroid. Note that a loose connective tissue capsule invests both parathyroid and thyroid but the parathyroid is outside the true thyroid capsule. The parenchyma comprises dense cords (closely spaced nuclei) of small (typically 8 – 12 um) chief cells . Loss of blood has created the artifactual appearance that the epithelioid cells are joined together in a homogeneous mass. Oxyphils, which are often clustered, are not evident in this particular section but can be seen in the next slide. Parathyroid chief cells can be confused with lymphatic tissue. However, note that the parathyroid cells have more cytoplasm and paler staining nuclei.
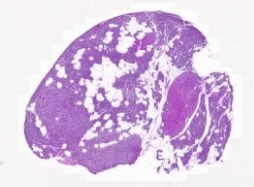
Webslide 0312_F: Parathyroid glan, human, H&E [DigitalScope] This section contains the same dense cords of relatively small chief cells as seen in the previous slide. In addition, there are a few clusters of larger (20 um) oxyphil cells with red staining cytoplasm. Characteristically, in adults the connective tissue septa become more evident with the addition of adipose tissue as seen in this slide.
Webslide 0062_F: Adrenal, monkey. H & E. Plastic [DigitalScope] The preservation of this slide is quite good, especially in the medulla. Capsule. Dense and cellular. Vessels superficially are arterioles of the capsular plexus which then feeds the parenchyma in broad capillaries. Note the adipose tissue outside the capsule. Cortex. Note the three distinct regions: Medulla. The abundant chromaffin granules are conspicuous. Different cells have different sized granules; this fact can be used to trace the outline of cells. Note that medullary cells in this slide intermingle in complex shapes.
Webslide UMich 230: Adrenal gland, human, H&E [DigitalScope] This slide exhibits the same features as above, although the human adrenal gland often has portions where there is only cortex and not much medulla (e.g. on the left side of the slide). In this specimen, one can also better appreciate the basophilic staining that is more typical of the chromaffin cells in the medulla. Recall that these cells are essentially postganglionic neurons that release epinephrine and norepinephrine into the bloodstream, and you should note these cells are quite similar to other neuronal cell bodies you’ve already seen in peripheral ganglia. Finally, note the large central (or medullary) veins that receive the secretions of the chromaffin cells and also drain the cortex, thus delivering hormones produced within this gland to the entire body via the bloodstream.
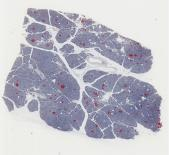
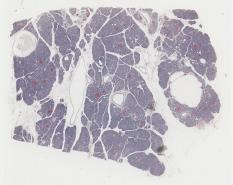
Webslide 0095_F: Pancreas, monkey. H&E, Plastic [DigitalScope] Survey the slide at low power, looking for groups of lightly stained cells, the islets of Langerhans. Roughly estimate the relative volume of acinar to islet tissue. Special stains are needed to distinguish the three principal cell types in islets. Note the large capillaries passing among the islet cells. Some artifactual dilatations are seen in the islet cells
Webslide MA102900: Pancreas, Insulin immunostain (courtesy of Univ. Tasmania) [DigitalScope] Webslide PA103905: Pancreas, Glucagon immunostain (courtesy of Univ. Tasmania) [DigitalScope] Slide MA102900 has been stained with an anti-insulin antibody that stains the beta cells of the islets dark red. A similar process was done to slide PA103905, except this time using an anti-glucagon antibody to label the alpha cells of the islets.
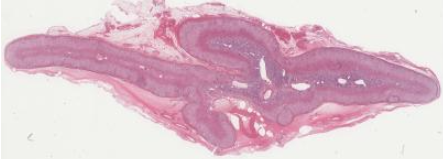
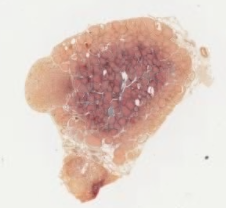
Pathology Correlate The slides below show a rodent thyroid at three different levels of functional activity:
Compare the tissue shown in each slide –the variation is not overwhelming since the experiments were performed conservatively, but you should be able to see some differences in epithelial cell height and in the size of the follicular lumens. Look first at the normal thyroid [DigitalScope] to get a baseline.
Hypoactive thyroid follicular cells [DigitalScope] Now, look at the hypoactive thyroid gland caused by removal of the pituitary gland (hypophysectomy). After hypophysectomy there is no stimulation by TSH, so the follicular epithelial cells become reduced in height and the colloid in the lumen is abundant, since it is not being resorbed to make thyroid hormones. In these hypoactive slides, C-cells [example] are more obvious as these cells are fully functional and not dependent on TSH. C-cells:
This particular example illustrates what would be observed in secondary hypothyoidism in which there is a failure of the anterior pituitary to produce adequate amounts of TSH. In most patients who have hypothyroidism, the issue is usually primary hypothyroidism, in which the issue is something directly affecting the thyroid itself --the most common cause is inflammation of the thyroid (thyroiditis) that causes it to not produce adequate amounts of thyroid hormone.
Hyperactive thyroid follicular cells [DigitalScope] This specimen shows how hyperactive follicles would appear. One possible cause of hyperactive follicles could be Graves disease in which autoantibodies bind to the TSH receptor on thyroid follicular cells and stimulate them to take up colloid and release active thyroid hormone. Alternatively, there could be a pituitary tumor that secretes high levels of TSH that activates the thyroid gland. Hyperactive thyroid cells:
However, the source of the pathology in this specimen is that the animals have been treated with thiouracil, which blocks the oxidation of iodide, the result of which is that functional thyroid hormones can no longer be produced. The lack of thyroid hormones in the blood stream leads to stimulation of the pituitary to produce large quantities of TSH, causing the thyroid follicular cells to hypertrophy and resorb colloid very actively from the lumen, reducing its size. The frantic effort of these cells is futile, however, since the oxidized iodine necessary to make functional thyroid hormones is unavailable. As such, the actual follicular cells are "hyperactive" in terms of actively taking up and processing thyroglobulin, but the thyroid status of this subject would be hypothyroid (i.e. low thyroid hormone levels). For this reason, it is essential to have lab values regarding actual thyroid function to go along with the microscopic analysis of thyroid tissue when working up patients with thyroid conditions. *sidenote about thiouracil - some plant materials, such as cassava root, contain compounds that are converted to thiocyanate that acts similar to thiouracil and are known causes of endemic goiters that can occur in some populations. What would be the appearance of the thyroid of a person with Graves disease?
Practice Questions 1. The parathyroid gland primarily regulates which of the following in the body?
2. Which cell type in the anterior pituitary is primarily responsible for the secretion of growth hormone?
3. The zona reticularis of the adrenal cortex is involved in the production of which hormones?
4. A 30-year-old man presents with symptoms of increased heart rate, sweating, and high blood pressure. Imaging reveals a mass in his adrenal gland. Which cell type is most likely involved?
5. A patient presents with fatigue and hypoglycemia. Lab tests show that he has low levels of both ACTH and cortisol. Which of the following best explains these findings?
Organ Review 0095_S [DigitalScope] Identify as specifically as possible the organ shown in the slide AND provide at least FOUR specific or characteristic features (e.g. specific cell types and/or arrangements of cells/tissues in the organ) supporting your identification. For EACH feature listed, provide a brief explanation regarding its functional significance and/or how that feature is helpful in terms of distinguishing the organ. [ANSWER]
Extra Slides I. PITUITARY GLANDThese slides show mostly pars distalis, but also have a small area of neurohypophysis (either pars nervosa or infundibular stalk) on one side (see slide orientation diagrams) and are stained in alternate sets with H&E or with Masson trichrome. The two classes of anterior pituitary cells (acidophils and basophils) are most easily distinguished with Masson trichrome staining, but you should also see how they look with routine H&E staining. A. Pars distalis (aka anterior pituitary or adenohypophysis)226 Pituitary gland, human, Masson cross [DigitalScope] Study the pars distalis (anterior lobe) in slide 226 stained with Masson trichrome. The cells are arranged in irregular clusters or cords and are distinguishable by their staining as either acidophils, basophils, or chromophobes. The acidophils stain red or orange-red, while the basophils stain various shades of blue or blue-gray. Remember that the acidophils include two different cell types, somatotropes (growth hormone) and mammotropes (prolactin), while the basophils include gonadotropes (FSH and LH), thyrotropes (TSH) and corticotropes (ACTH). ACTH is actually a cleavage product of pro-opiomelanocortin (POMC), which is made by corticotropes and processed primarily into ACTH in these cells. To a lesser extent, corticotropes also produce other signaling factors derived from POMC such as lipotropins (involved in lipid metabolism), endorphins (endogenous opioids that reduce pain perception), and melanocyte stimulating hormone (MSH). Depleted or immature secretory cells of the anterior pituitary show no distinctive staining and are called “chromophobes”. The cell types are not uniformly distributed throughout the pars distalis, but instead there are areas where acidophils predominate, other areas where basophils are more numerous, while still other regions may show a more even mixture of acidophils and basophils. As you identify these cell types, keep in mind that most histological surveys find that 50% of the overall cells in the anterior pituitary are chromophobes, 40% are acidophils, and only 10% are observed to be basophils. Note the abundant sinusoidal capillaries (often filled with red blood cells) that lie between the cell cords or clusters. You can appreciate how readily the hormones secreted from the cells can reach the blood. Since collagen stains bright blue with the Masson trichrome method, you can see the delicate connective tissue partitions between cords and around blood vessels. In the routine H&E-stained sections, you can also identify acidophils and basophils, although the difference is not as obvious as it is with Masson trichrome staining. Here again, you should first identify acidophils, which stain various shades of reddish pink, and then the remaining cells are almost entirely basophils, which vary generally from bluish/grayish-pink to blue. B. Pars nervosa (aka posterior pituitary or neurohypophysis)227 Pituitary gland, monkey, Masson cross [DigitalScope] Although the pars nervosa can be found on the human pituitary slides in our collection, the monkey pituitary specimens (H&E and trichrome-stained) contain a significant portion of the pars nervosa (posterior lobe) and are probably better for studying this tissue. The pars nervosa looks like brain tissue, which it is. It is an extension of the brain, composed primarily of nerve fibers (axons) which originate from nerve cell bodies in the hypothalamus and pass to the pars nervosa by way of the hypothalamo-hypophyseal tract and the infundibular stalk. These nerve fibers carry oxytocin and antidiuretic hormone (ADH, vasopressin) to nerve endings, from which they are released into nearby capillaries upon neural stimulation from the hypothalamus. There is not much to see in the posterior lobe in these histological sections. Since there are no neuron cell bodies in this structure, most of the prominent nuclei belong to pituicytes , which are the characteristic glial cells of the pars nervosa. You will also see the nuclei of blood vessel endothelial cells , and fibroblasts which are in the connective tissue around these vessels. C. Pars intermedia227 Pituitary gland monkey, Masson cross [DigitalScope] The pars intermedia is very poorly developed in the human pituitary, but is prominent in the pituitaries of most other mammals. For example, in the monkey pituitary, you will see the pars intermedia as a prominent layer several cells thick, lying between the pars distalis and pars nervosa. In some places you may also see a long cleft between the pars distalis and the pars intermedia, which is a substantial remnant of the lumen of the embryonic Rathke’s pouch, an ectodermal outpocketing of the oral cavity which gave rise to both the pars distalis and the pars intermedia. Cells of the pars intermedia also produce POMC (pro-opiomelanocortin), which in humans is processed primarily into endorphins and lipotrophins. In contrast to its substantial presence in other mammals, the pars intermedia of the human pituitary is usually represented merely by a thin layer of basophilic cells that can be seen in both the human trichrome and H&E-stained human sections lying against the pars nervosa, and is probably of little functional importance. Between the pars intermedia and pars distalis are occasional fluid-filled cysts (again visible in both trichrome and H&E-stained sections), which are the only vestiges of the lumen of Rathke’s pouch. Although most of the human axial sections in your sets do not show the human pars intermedia very well, the sagittal sections in some of the sets show some indication of it. D. Infundibular stalk and hypophyseal portal vessels229B Infundibular stalk, and hypophyseal portal vessels H&E [DigitalScope] This slide shows the hypophyseal portal blood vessels that carry releasing hormones from the hypothalamus to regulate the release of hormones from the pars distalis of the pituitary. Look for these prominent blood vessels in portions of the pars distalis that extend up around the infundibular stalk. In many of these slides the sinusoidal capillaries lying between cords of pituitary cells throughout the anterior pituitary are shown particularly well. Scan over the slide, reviewing other features you saw in slides 226 and 227 (e.g. acidophils vs. basophils; neurohypophysis vs. adenohypophysis).
II. THYROID GLAND217 Thyroid gland, parathyroid H&E [DigitalScope] Examine slide 217 at low magnification, then at higher magnifications. Note that the thyroid gland is made up of functional units called follicles, which in three dimensions are approximately spherical, their walls being composed of a simple cuboidal epithelium, surrounding a lumen that contains colloid. Note that the follicles vary in size and that the height of the follicular epithelial cells may also vary. The colloid is composed primarily of thyroglobulin, a glycoprotein synthesized by the follicular epithelium. Under stimulation from pituitary TSH, the thyroid cells break down the thyroglobulin to release thyroid hormones (T3 and T4), which pass into nearby capillaries. Occasional parafollicular cells (C-cells), source of the hormone calcitonin, are also present between the follicles and in the follicular epithelium. However, they are difficult to distinguish in routine histological slides of human thyroid, and you are NOT expected to recognize them based on light microscopy alone (but you should know that they are the source of calcitonin which is packaged into secretory granules that makes these cells readily identifiable by electron microscopy).
III. PARATHYROID GLAND217 Thyroid gland, parathyroid H&E [DigitalScope] Sections of parathyroid gland can be seen on slides 217, 220, and 221. In slide 217, parathyroid tissue will be found on one side of the much larger mass of thyroid tissue. To find the parathyroid tissue on slides 217, scan around the periphery of the thyroid tissue at low magnification. The parenchyma of the gland is made up of two identifiable cell types: the predominant chief (or principal) cells (source of parathyroid hormone) and occasional oxyphil cells. Observe the arrangement of chief cells in the parathyroid as seen on slides 217, 220, and 221. The chief cells are arranged as interconnecting cords or clusters, with blood vessels and connective tissue forming the partitions between the cell cords. The capillaries in slide 221 may be more easily seen because erythrocytes have been retained within the lumens. The individual chief cells, seen well in slide 220, have relatively little cytoplasm, which may be almost unstained or lightly basophilic. The lightly stained cells are thought to be quiescent while the more basophilic cells are believed to be more actively involved in the synthesis and secretion of parathyroid hormone. In either slide 217, 220, or 221 try to find oxyphil cells. Oxyphil cells are much less numerous than chief cells, and can be differentiated from them by the following criteria: (1) larger than chief cells, with more extensive, eosinophilic cytoplasm, (2) nuclei smaller and darker staining, (3) usually occur in isolated groups. The exact function of these cells is unknown, but they are unique to the parathyroid gland and therefore helpful in identifying it.
IV. ADRENAL (Suprarenal) GLANDSlide 230 (adrenal gland, human, H&E) [DigitalScope] At low magnification on the human adrenal gland (slide 230), note that the gland is enclosed by a connective tissue capsule and has two principal regions - a cortex and a medulla. The cortex occupies the greatest area on your slide. In many regions of slide 230 you will see only cortex, because some parts of the human adrenal lack medulla. The cortex is made up of three regions or zones: the zona glomerulosa, the zona fasciculata and the zona reticularis. The zona fasciculatais probably the easiest layer to spot as it is a broad zone of cells arranged in straight cords, one or two cells thick, which run at right angles to the surface of the gland. The cells of the fasciculata are lightly stained and have a frothy appearance, due to the extraction of lipid droplets from the cell cytoplasm during tissue processing. Interior to the fasciculata is the zona reticularis, which stains more deeply than the other two regions of the cortex. The cells of the zona reticularis are arranged as anastomosing (reticular or net-like) cords. The zona glomerulosais found outermost in the cortex and consists of cells arranged in rounded or arched clusters although in the human adrenal gland, the zona glomerulosa may not be present around the entire periphery of the cortex. In other species, however, this zone exists as a complete layer around the entire periphery of the cortex as shown in slide 231, which of the monkey adrenal gland. Continuing inward on slide 231, you should be able to recognize the zona fasciculata, zona reticularis, and, finally, medulla. Notice that throughout the cortex of both the human and monkey adrenal glands are numerous capillaries, with somewhat expanded lumens. Return to the medulla of slide 230 (human adrenal section). The medullary cells, source of norepinephrine (noradrenalin) and epinephrine (adrenalin), are often more basophilic than the cells of the cortex.The cells of the medulla are considered to be modified postganglionic sympathetic neurons (derived from neural crest cells). These secretory cells are also called chromaffin cells, because their secretory granules (containing norepinephrine or epinephrine) stain brown with potassium dichromate. Note the branches of the central (or medullary) vein in the medulla, and review the blood circulation of the adrenal.
|
|||